Dave Bunting
As we are now emerging from the Covid-19 era, it is time to reflect on the challenges and opportunities that the pandemic has brought. Hospital trusts have had to endure staff sickness/shortages, bed crises and severely reduced operating capacity, all of which have impacted hugely on our day-to-day work. Hospitals have had to find new ways of safely providing surgical care during the ongoing pandemic and day surgery units have played a huge part in restoring our elective and urgent care services to keep up with ongoing demand and deal with the inevitable waiting list backlog that has developed in most specialties. Day surgery units, being naturally separated from inpatient bed facilities and with their own admission and discharge routes are ideally equipped to facilitate so-called ‘green’, low-Covid risk pathways for patients to be treated without impacting on emergency and inpatient facilities. The importance of securing ring-fenced beds for day case activity has been clearly demonstrated. The drive to reduce inpatient bed occupancy and manage patients on an ambulatory basis promises to build momentum and further push the boundaries of day surgery. The recent BADS Virtual Conference held in March – ‘Using Day Surgery to Recover Elective Surgery in the Era of Covid-19’ - presented excellent examples of novel practice in day surgery that will change the way we treat many conditions traditionally managed with inpatient surgery across many surgical specialties. In Urology, we have learned how many cases of benign prostatic hypertrophy and ureteric stones can be managed in outpatient and day surgery environments using novel techniques. Similarly, in gynaecology, hysteroscopy and endometrial ablation are being increasingly performed in outpatients and many units are regularly performing procedures such as anterior repair, vaginal hysterectomy, and laparoscopic hysterectomy as a daycase. In orthopaedics, anterior cruciate ligament repair, total knee replacement and total hip replacement are being performed regularly as day surgery in several trusts. Even urgent procedures classically performed with inpatient stays such as laparoscopic cholecystectomy for acute cholecystitis/pancreatitis and open reduction and internal fixation of mandibular/zygomatic fractures are now routinely being performed on an ambulatory basis.
All material presented at the BADS Virtual Conference including video recordings of invited speakers’ lectures and oral prize presentations will be available online for registered participants to access free of charge for 3 months following the conference.
In this edition of JODS, three updated ‘How I do it’ day case guides are presented, including guides on Laparoscopic fundoplication, Vaginal hysterectomy & Vaginal repair and Tonsillectomy. Scientific articles this month include a review of anaesthetic factors that may contribute to overnight stays in anterior cruciate ligament reconstruction and a description of a rare skin cancer treated with serial day surgery attendances.
As usual there are pages dedicated to events of educational interest including the BADS / HCUK Conference on Day Surgery Gynaecology which is due to take place very soon on Thursday 20th May – there is still time to register for this virtual meeting with a discounted rate of £100 + VAT for trainees and BAD members.
Please keep your submissions to the journal coming in and remember – JODS still offers citable peer-reviewed publication with no author processing fees. Updated author guidelines and submission instructions can be found in this edition of the journal.
Finally, I cannot let this edition pass without highlighting that it is the final edition to be published with BADS led by our President Kim Russon. Kim took on the role at short notice and from the very start has demonstrated a huge commitment to the organisation. BADS is a fantastic organisation with a bright future - credit for which must go to Kim who has led the organisation through huge changes and challenges with regards to the RCS Eng rebuild and the Covid-19 pandemic. As a leader, she has a manner which is diplomatic, considered, non-judgemental and sensitive to individuals - I am not sure whether this is conscious / learned or whether it is just her natural way - but I know that we could all benefit from some of that wisdom. With that said I look forward to reading her final President’s letter and would like to personally thank Kim for her devotion and enthusiasm over the past two years.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50188/312-editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse0

Kim Russon
I hope this finds you all safe and well. The last few months have continued to be challenging but things do seem to be improving. The UK vaccination programme is progressing well, enabling the government to relax restrictions and offering people the opportunity to meet up with friends and family and hopefully to go on holiday and get some well deserved rest. Variable progress has been made nationally to reduce the elective surgery waiting lists but thankfully there does seems to be some appetite to help address this by different ways of working rather than “just doing more” which should be recognised as being potentially detrimental to staff well being. One solution is to manage more surgery using day case pathways and BADS continues to work with Get It Right First Time (GIRFT) and NHS Integrated Care Systems (ICS) to promote and progress this.
How to use day surgery to help recover elective surgery was the focus of our recent BADS virtual conference. What a totally fabulous conference! So much information delivered slickly in one day. I must thank the conference team, AV company and all of our superb speakers and the delegates who attended and helped to make it such a huge success. We were privileged to have so many high quality speakers sharing examples of what can be performed as a day case. Don’t worry if you missed it, the recording is still available for BADS members to watch via our BADS website.
I am delighted to report BADS membership has grown and the Society now has over 550 members. BADS is committed to developing and promoting day surgery and to support our members to do this. With this is mind, we have plans to increase the resources available to members on the website, so please keep a look out! The new BADS website was launched in March 2021 and I hope you are all enjoying the new look as much as I am. Available on the website later this year will be a list of day surgery leads and managers to enable BADS members to be able to contact each other and share knowledge and expertise and also assist BADS to keep day surgery units up-to-date of national developments. If you are a day surgery lead and happy to be part of this then please contact bads@bads.co.uk
Following excellent delegate feedback from our joint conferences, BADS continues to collaborate with Healthcare conferences (HCC) to deliver one day speciality focused conferences where teams achieving successful day surgery share their knowledge and pathways to enable other centres to learn how to deliver similar services.
- Day Surgery in Gynaecology 20th May 2021
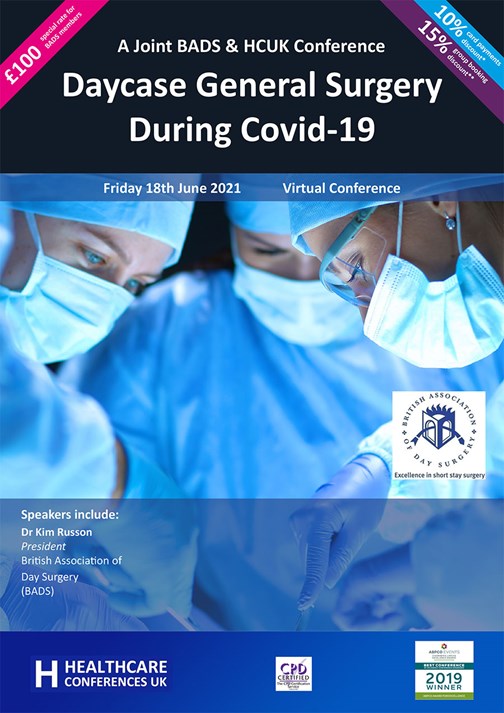
- Day Case General Surgery During Covid 18th -19th June 2021
- Day Case Urology 8th July 2021
- Breast Surgery as Day Surgery 7th Sept 2021
- Daycase Major Knee Surgery 4th November 2021
- Day Case Total Hip Replacement 18th November 2021
I was saddened and slightly surprised when I initially realised that this is my final President’s letter for JODS. The past two years have flown by! However, when I reflect on the achievements we have made over the last 2 years I feel very positive: we have strengthened the BADS governance processes, moved over to virtual council meetings, delivered a number of virtual conferences, grown the membership and significantly raised awareness of day surgery nationally. I am so proud of how much day surgery seems to have moved forward over the past few years. I have been supported by an excellent council to whom I would like to expressive my immense gratitude. BADS could not do what it does without the hard work and dedication of council. I would like to specifically thank Nicola Adams, BADS administrator for all of her help and patience during my Presidency. Nicola is the backbone of the Society and it couldn’t run without her. She has given a vast amount of additional time to enable BADS to deliver the BADS virtual conference and the new BADS website.
BADS council sadly have two farewells. Janet Mills has been the BADS Exhibition manager for over 14 years. Her easy going, friendly manner drew many exhibitors to support BADS annual conference year after year and she will be missed by council. Thank you Janet and please enjoy your retirement! Someone else who will leave an enormous gap is immediate past President Mary Stocker. She has been on Council for over 11 years and has also been Conference secretary and Treasurer. She has been a huge driver of day surgery locally and nationally and offered invaluable support and guidance to me personally and to BADS council. I am sure Mary’s enthusiasm and drive to progress day surgery will continue. Thank you Mary from me personally and on behalf of BADS.
Council elections are currently in progress and I am delighted to report that we have received 5 expressions of interest to join BADS Council (2 are current council members seeking re-lection). The biographies of Mrs Alex Alen, Mrs Fiona Belfied, Mr Muhammad Rafaih Iqbal, Dr Joellene Mitchell and Dr Rachel Tibble are available to view on the BADS website. All BADS members should have received a link to be able to submit their vote. Voting will close on 28th May 2021.
I shall be handing over the BADS Presidency to Miss Jo Marsden at the BADS Virtual AGM on Friday 9th July 2021. Jo has a great passion for day surgery and I’m sure will lead the Society well. Thank you again to everyone for their support and contribution to day surgery, please take care and I hope you can join us at the virtual AGM.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50189/312-pres.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse1
Ian Finlay, Consultant Upper GI, Bariatric, Laparoscopic and General Surgeon
Royal Cornwall Hospitals NHS Trust
Patient Selection
- Standard day case criteria
- Hiatus hernia containing less than half of stomach
Anaesthetic Techniques
- Standard day case protocol GA:
- Rapid sequence ET induction with propofol, rocuronium, fentanyl
- Maintenance with sevoflurane (avoid nitrous oxide), or propofol TIVA if higher PONV risk
- 3 anti-emetics given intraoperatively (ondansetron, dexamethasone, cyclizine or droperidol) with fourth as reserve for use in recovery if needed
Surgical Technique
- Patient legs straight and apart, slightly head up, surgeon between legs with assistant on patient's left
- 1 x 12mm camera port, 3 x 5mm working ports, suture passed via camera port. Diamondflex liver retractor via right side 5 mm port
- 12mmHg CO2, dissection with Lotus ultrasonic energy device
- 360o Nissen or 180o anterior fundoplication as per surgeon's preference
Peri-operative Analgesia
- Fentanyl titrated intra operatively (250 – 500mcg)
- 20ml of 0.5% levobupivacaine to port sites at end of case
- Avoid morphine, fentanyl in recovery, Oramorph only if required
Take Home Medication
- Prochlorperazine 3mg buccal tablets - 1-2 twice daily for 2 days PRN
- Over the counter soluble paracetamol and ibuprofen - pre op' purchase advised
Organisational Issues
- Patients advised pre op' that day case procedure normal practice
- First on list to allow longer recovery before discharge
- Telephone call from Specialist Nurse first day essential for reassurance
Common Pitfalls
- Day one increase in dysphagia (inform of this pre op')
- Pain worse if analgesia taken PRN instead of regularly
Anticipated Day Case Rates
- >80%
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50190/312-lapfund.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse3
Dr Mary Stocker, Consultant Anaesthetist
Mr Naru Narayanan, Consultant Gynaecologist
Torbay and South Devon NHS Foundation Trust
Patient Selection
- All women who need surgical treatment of prolapse
- No exceptions
- All surgeons working to the same protocol
Anaesthetic Techniques
- General or Spinal Anaesthesia
- General Anaesthesia
- Induction and maintenance with target controlled propofol and alfentanil infusions.
- Spontaneous ventilation with Laryngeal Mask Airway
- Spinal Anaesthesia
- 3mls 2% hyperbaric prilocaine
- All Cases
- Always give 1 litre crystalloid as this reduces PONV and dizziness: usually do not need more than this.
- IV Dexamethasone 6.6mg and ondansetron 4mg iv for hysterectomies
- Anti-emetic medication is not routinely required for vaginal repair surgery
- Subcutaneous fragmin 5000u at end of procedure if >60 minutes
Surgical Technique
- Lithotomy position.
- Infiltration with 0.25% Bupivacaine and 1:200000 adrenaline. 20mls per compartment.
- If hysterectomy, then I use finger switch diathermy to make incisions.
- I ensure meticulous haemostasis.
- Mostly 3 pedicle hysterectomy
- If uterine size more than 12 weeks pregnancy size, then I will bisect the uterus after taking the uterine pedicle to make it easier to place a clamp around the cornual pedicles.
- No pack and no catheter as routine.
Peri-operative Analgesia
- Pre-medication with oral Ibuprofen Retard 1600mg and Paracetamol 1g.
- Intra-operative iv fentanyl 25mcg prn.
- Post-operative iv fentanyl prn, then oramorph and regular paracetamol.
Take Home Medication
- Paracetamol 500 mg/ codeine 30mg po qds, laxido 1 sachet bd, plus ibuprofen 400 mg po qds
Anticipated Day Case Rates
- > 80%
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50191/312-vaginal-hysterectomy.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse4
Jane Montgomery & Shyam Singham
(Original article published 2013, updated 2020)
Patient Selection
- Age 3 and over
- Caution in patients with severe sleep apnoea
- Within 30 mins drive of hospital
- Transport in own car
Anaesthetic Techniques
- EMLA or Ametop cream
- Propofol 4mg/kg
- Disposable reinforced LMA (a size down from what you would otherwise use) size 2 if <20kg
- Maintenance with isoflurane or sevoflurane in air and oxygen
- Spontaneous respiration
- Dexamethasone 0.25mg/kg
- Ondansetron 0.1mg/kg
- Crystalloids 10ml/kg
- In recovery free fluids and food on demand
Surgical Technique
- Coblation surgical technique to reduce PONV with decreased per-operative bleeding
- 5% lignocaine with phenylephrine spray to tonsillar beds at the end of surgery
Peri-operative Analgesia
- Preoperative ibuprofen 5mg/kg
- Preoperative paracetamol 15-20 mg/kg
- IV Fentanyl 1-2mcg/kg intraoperatively
Take Home Medication
- Azithromycin 10mg/kg for 3 days od
- Ibuprofen 5-10mg/kg for 1 week qds
- Paracetamol 15mg/kg qds for 1 week qds
Organisational Issues
- Nursing observations for 6hrs postoperatively
- Nurse led discharge 6hrs postoperatively so need to be on morning list
- Surgeon needs to be contactable in the afternoon if there are any concerns
Common Pitfalls
- Site rLMA in anaesthetic room and do not tape to mouth. Check airway patent with head in extension to mimic surgical position
- Ensure surgeon uses relatively large Doughty blade to avoid compression of rLMA on posterior third of tongue base
- When gag is put in, if the surgeon can see rLMA cuff it’s not far enough in
- Insertion of gag initially can induce apnoea momentarily—check airway patent with brief bagging
- If still a problem release gag and put a little tension on the rLMA as it is replaced (may
stop rLMA folding on itself). Sometimes the obstruction is relieved when the surgeon places the Draffin rods - If still a problem revert to RAE endotracheal tube
Anticipated Day Case Rates
- 95%
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50192/how-i-do-it_tonsillectomy.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse5
Stamatios Karavolos, Consultant Gynaecologist, Salford Royal NHS Foundation Trust, BADS Council Member
Thursday 19th of November 2020 saw the first joint British Association of Day Surgery (BADS) and Healthcare Conferences UK (HCUK) one-day conference titled “Developing a Daycase Gynaecology Surgery Service”. The conference provided a unique opportunity to virtually meet with pears from the across the UK that came together on a virtual platform, for what promised to be an educational and thought-provoking conference, very topical in the era of the COVID-19 pandemic.
The conference was chaired by BADS council members Dr Mary Stocker, Consultant Anaesthetist, Torbay and South Devon NHS Foundation Trust, Past BADS President and Dr Stamatios Karavolos, Consultant Gynaecologist, Salford Royal Hospital, Manchester. This conference heard the experiences of teams from different Trusts in the UK that have successfully implemented their day case pathways, the key to their success and ways to overcome any obstacles.
Dr Stocker, who chaired the morning session, introduced the newly published BADS ‘Day Case Gynaecology Surgery’ handbook, the latest addition to a series of handbooks published by BADS. This is now available to purchase from the BADS website.
The first talk was delivered by Dr Stocker, who presented on key aspects of the day case pathway and ways to implement it. Quality improvement was discussed, as well as how to measure outcomes and success. She also touched on national figures for day case gynaecology procedures as highlighted in the 2020 Getting it Right the First Time (GIRFT) national programme that addresses national variation on day case services. Her talk was followed by two presentations on specific procedures done as day case. Mr Jonathan Hindley and Mr Naru Narayanan, Consultant Gynaecologists at Torbay and South Devon NHS Foundation Trust, shared their experience with day case laparoscopic hysterectomy and day case vaginal prolapse surgery, respectively. Both speakers discussed key aspects of patient selection and surgery techniques that help make day surgery successful. The morning session concluded with a talk from Sister Alex Alen, Torbay and South Devon NHS Foundation Trust, who elaborated on the practicalities and key aspects of the pre-operative assessment that are important for a successful day surgery pathway.
The afternoon session started with a talk from Dr Peter Scott, Consultant Gynaecologist at the University Hospital of Plymouth, with title: ‘Taking a step further to moving procedures down the intensity gradient into the outpatient clinic’. Dr Scott discussed his experience with moving an number of procedures to the outpatient setting. He established a successful outpatient hysteroscopy/menstrual disorders clinic performing procedures such as endometrial ablation and manual vacuum aspiration (MVA) in the outpatient setting. He discussed the challenges he faced in setting up this clinic and ways to overcome them. Following this Dr Nicola Ramsaw, senior trainee at Northumbria Healthcare Trust, shared her experiences of running a day Case gynaecology service at Northumbria, one of the leading day case surgery units in the country that have achieved up to 92% day case total laparoscopic hysterectomy rates. Dr Ramsaw outlined the patient pathway and general principles for day case surgery pathway that have enabled her unit to achieve these impressive results. This was followed by Dr Theresa Hinde, Consultant Anaesthetist at Torbay and South Devon NHS Foundation Trust and BADS honorary secretary, who talked on her experience in developing an emergency ambulatory gynaecology day case pathway and the importance of a collaborative approach with managers and clinicians from other specialties in order to successfully implement this. The conference concluded with a talk from Dr Stocker who summarised ways improve day surgery gynaecology services using the model hospital tool for auditing and monitoring outcomes.
A big thank you to all the speakers, delegates and organisers who made the first day case gynaecology conference so successful. The next day case gynaecology conference is due to take place virtually on 20th May 2021.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50193/312-developing-a-day-case-gynaecology-surgery-service.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse6
Dr Amy Thomas, Consultant Anaesthetist, The Rotherham NHS Foundation Trust
I enrolled on this conference to build on my existing experience of day case arthroplasty, and nosy at other centres’ successful techniques. We all know there are several ways to “skin a cat” but I wanted to know how to do it well! This conference did not disappoint. There was a variety of speakers representing the multidisciplinary team from various UK Trusts. They fielded questions live in the Question & Answer sessions, via the online chat facility and by email following the sessions.
Mary Stocker’s talk on “optimising day case surgery” inspired me to advertise more to Primary Care and start the “day case arthroplasty” message early in the patient’s journey. Her later talk on monitoring outcomes introduced me to the ‘BADS National Dataset’ which will help me understand my Trust’s National position better. She improved my familiarity with Model hospital and the info it will yield!
Hiren Divecha from the Wrightington talked about “Undertaking your first day case hip replacement”. A really engaging talk that involved a patient giving their feedback. For me it highlighted the value of enhanced recovery nurses throughout the patient’s journey. We currently do not have this role in our Trust but during the conference it was a common theme and seems to be the way forward as we expand the complexity of operations performed.
Claire Blandford and Mike Kent presented work from Torbay’s successful day case arthroplasty service. A pragmatic talk which I enjoyed and learnt lots from. They demonstrated how adhering to a protocol increases successful discharge rates stating we should aim for 20% of our total hip replacements to be performed as day case. New practice to take forward in my hospital will be the inclusion of carbohydrate drinks in the preoperatively and postoperatively and the administration of two doses of tranexamic acid. I think cell salvage collection for all will spark debate at home. I particularly like the patient TTO (to take out) drug charts to help patients monitor their own medication after discharge.
Northumberland’s recipe for success was very different to my own experience and thought provoking. They presented their relatively opiate-light technique using regular mobilisation to reduce pain postoperatively. This has been enabled partly with the “Taurus walker” and the consensus that hip precautions should be consigned to history. It was a shame Hilary wasn’t available for questions on the day. I suspect their use of high dose dexamethasone (8-16mg) will help their pain scores.
Ed Dunstan presented Scotland’s Model which evolved after a trip to see the work in Copenhagen. They also have seen a ripple effect; increasing day case rates reduces the overall length of stay in their inpatient population. Their use of general anaesthesia as standard was reassuring and I will take forward in my own practice. They are the only UK centre regularly using oral ephedrine to help prevent hypotension postoperatively. In addition, they routinely use high dose dexamethasone (24mg).
Steve Young’s work in Warwickshire developing a SWATT team has not only improved day case success rates but also highlighted long stayers that can be targeted for early intervention. SWATT discussion of all failed day cases has helped them evolve their practice. Their online patient education preoperatively caught my eye, a leap our Trust need to make!
Take-home messages of the day for me:
- Carbohydrate drinks pre- and post-operatively prevent hypotension on mobilisation
- Prilocaine or Bupivacaine 0.25% spinals or GA are effective
- High dose dexamethasone
- Repeat tranexamic acid doses administration at the end of surgery
- Local anaesthetic infiltration of all cut surfaces
- Experienced and motivated teamwork with clear messaging
- Enhanced Recovery nurses pre- and post-operatively to help drive change
- Limit the doses of oxycodone for discharge medication, i.e., 3 to 5 individual doses
Please note that this conference will be held again on 18th November 2021.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50194/312-bads-hcuk-virtual-conference-report-daycase-total-hip-replacement.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse7
Hull, Frederick (Foundation Year 2), Huckle, Anthony (Foundation Year 2) & Thanawala, Vishal (Consultant Anaesthetist). Nottingham University Hospitals NHS Trust.
Author Contact: f.hull@nhs.net
Keywords
Anterior cruciate ligament repair; local anaesthetic infiltration; analgesia
Abstract
Introduction: The service level report generated by GIRFT (Get It Right First Time) showed that the average length of stay (LoS) for Nottingham University Hospitals (NUH) Trust following Anterior Cruciate Ligament Repair (ACLR) from April 2017 to March 2018 was 1.35-days. Reducing our LoS to match the national average of 0.13-days could save an estimated £45,000. We performed a review of anaesthesia and specifically postoperative nausea and vomiting (PONV) and pain as factors which may be contributing to our increased LoS to enable us to formulate perioperative guidelines.
Methods: 113 patients underwent ACLR in NUH between March 2018 and March 2019. Pain and PONV scores were analysed from recovery and at six-hourly intervals postoperatively using electronic observation data along with analgesic and antiemetic regimes used intra and postoperatively.
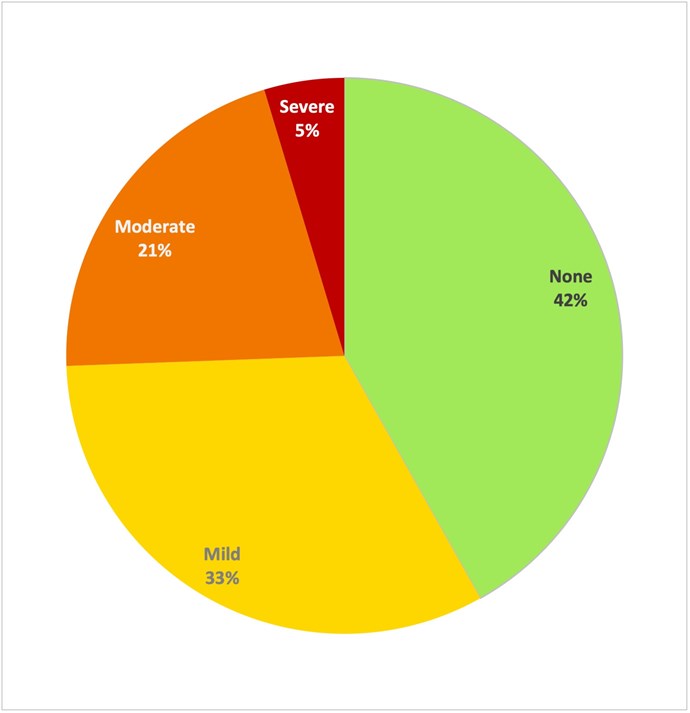
Results: Forty-seven patients (42%) experienced moderate-severe pain in the recovery room and 12 and 11 patients (11%, 10%) at 6 and 12-hours, respectively [Fig. 1-3]. Four patients (3.5%) received intraoperative local anaesthetic infiltration, and 13 patients (12%) received a femoral or adductor canal nerve block.
Conclusion: Use of intraoperative local anaesthetic infiltration/nerve block has been shown to improve pain control for up to 24-hours in ACLR [4]. We recommend use of local anaesthetic infiltration or regional anaesthetic nerve block for all patients as well as use of multi-modal postoperative analgesia consisting of paracetamol, NSAID’s and an opioid as part of the discharge medication for the first 48-hours to provide optimal analgesia and facilitate day case surgery. We are in the process of formulating day surgery pathways and guidelines to reduce inpatient stay, improve patient experience and save revenue for the Trust.
Introduction
The GIRFT (Get It Right First Time) report for 2017-18 showed that the average length of stay (LoS) for patients undergoing anterior cruciate ligament repair (ACLR) at Nottingham University Hospitals NHS Trust was 1.35 days. Reduction in the LoS to match the national average of 0.13 days can help save an estimated £45,000 annually, according to local trust data. Postoperative nausea and vomiting (PONV) and pain were evaluated as potential anaesthetic factors contributing to delayed discharge.
Aims
- Determine the number of patients operated as day cases.
- Determine the incidence of PONV and severity of pain.
- Evaluate the perioperative analgesia and antiemetic regimes.
- To recommend changes in practice to help facilitate day surgery for this group of patients.
Methods
Following ethical approval from the hospital clinical audit and quality improvement team, retrospective data collection was performed for all patients who underwent ACL repair from April 2018-March 2019. Digital Health Record (DHR) and Medway hospital data systems were used to gather data pertaining to perioperative analgesia and antiemetic drug usage from the anaesthesia booklet and the drug chart. PONV was classified as either absent or present and pain scores were rated as absent, mild, moderate, or severe.
Results
- 113 patients underwent ACLR in NUH between March 2018 and March 2019 and all of them (100%) were carried out as inpatients. 101 patients (89%) were discharged the next day, 11 patients stayed for two nights (9.7%), and one patient stayed for three nights (0.88%).
PONV:
- Two patients (1.8%) reported PONV in the recovery room, 10 patients (9%) at six-hours and two patients (1.8%) at 12 and 18-hours postoperatively. None of the patients reported PONV at 24-hours.
- Intraoperative antiemetic usage was as follows:
- 95 patients (84%) received ondansetron
- 61 patients (54%) received dexamethasone and
- 49 patients (43%) received cyclizine.
- Postoperatively, ondansetron, cyclizine, prochlorperazine and metoclopramide were used.
Pain:
- Forty-seven patients (42%) experienced moderate-severe pain in the recovery room, 12 patients (11%) at six-hours, 11 patients (10%) at 12-hours, three patients (2.9%) at 18-hours and 11 patients (26%) at 24-hours postoperatively.
- Intraoperative analgesia usage was as follows:
- 95 patients (84%) received paracetamol
- 98 patients (87%) received morphine or oxycodone
- 83 (73%) received an NSAID. NSAID’s used intraoperatively included either naproxen or parecoxib or diclofenac.
- Multimodal pharmacological analgesia (MMPA) was deemed to be a combination of paracetamol, NSAID and a long acting opioid.
- Of the 65 patients who were in none or mild pain in recovery, 45 (69%) received MMPA.
- Of the 47 patients who reported moderate-severe pain in recovery, 29 (62%) received MMPA.
- 13 (12%) patients received a nerve block with nine (69%) of these being femoral nerve blocks and the remaining four (31%) adductor canal nerve blocks.
- Six patients (46%) who received a nerve block were in moderate-severe pain in the recovery room and one patient (20%) was in moderate-severe pain after 24-hours.
- Four patients (3.5%) were documented to have received local anaesthetic infiltration; in recovery two of these (50%) reported moderate pain, one (25%) mild pain and one (25%) had no pain.
Figure 1. Percentage of patients reporting PONV (blue) and moderate-severe pain (red) at 6-hr
intervals following ACLR.
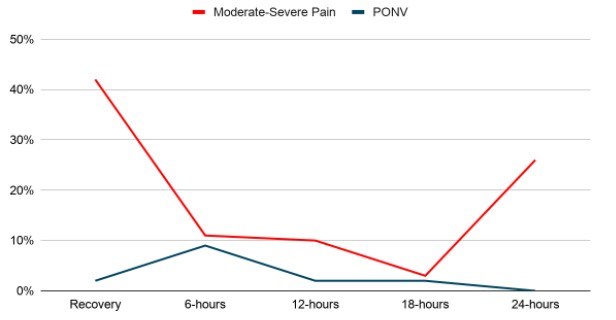
Figure 2. Pain scores (categorised by intensity) in recovery room post-ACLR. (n=112).
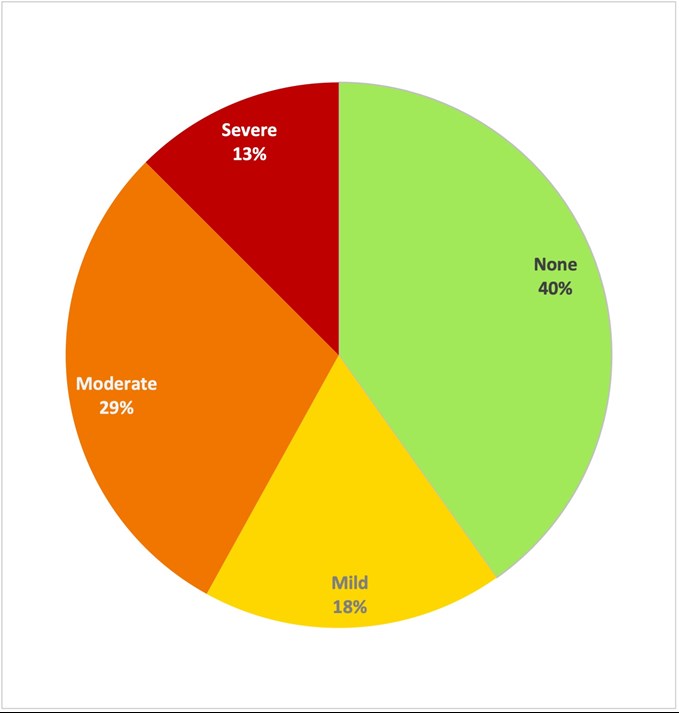
Figure 3. Pain scores (categorised by intensity) at 24hrs post-ACLR. (n=44).
Discussion
Our project aim was to identify potential anaesthetic factors which may contribute to delayed discharge for patients undergoing ACLR. The incidence of PONV was low peri-operatively, however we would like to suggest that all patients should receive at least two anti-emetics intraoperatively as per the departmental guidelines to reduce the potential incidence even further and enable timely discharge.
Postoperative pain was identified as a potential factor since 42% of patients reported moderate-severe pain in the recovery room and 26% of patients remaining in hospital experienced it at 24-hours postoperatively. Review of local nerve block usage showed that 12% of patients received a nerve block and 3.5% received local anaesthetic infiltration, albeit discussion with surgical colleagues suggests local anaesthetic infiltration was used for the vast majority of patients but it may not have been documented.
Several systematic reviews have been conducted into the efficacy of different regional analgesic techniques in ACLR operations (1, 2, 3). A recent literature review has recommended the use of multimodal analgesia in combination with local anaesthetic infiltration or addition of adductor canal nerve block in those patients at risk of severe pain (opioid tolerance, chronic pain) (4).
Limitations of this audit include that pain and PONV scores were recorded at a single point in time and may not fully represent the patients’ symptoms. The postoperative analgesia plan must be tailored for each patient individually taking into consideration their background comorbidities and opioid usage.
Overall, we suggest the use of local anaesthetic infiltration or adductor canal nerve block for all patients as part of multi-modal postoperative analgesia regime, in line with recommendations from the ACLR National Day Surgery Delivery pack (Appendix A) to ensure patients are comfortable in the postoperative period. The discharge analgesia prescription should include paracetamol, NSAID and a strong opioid for the first 48-hours to provide optimal analgesia.
We envisage that this audit will act to mitigate and minimize potential anaesthetic factors which contribute to delayed discharge and at the same time appreciate and understand the need of a multidisciplinary approach to address other non-anaesthetic causes. We have discussed the postoperative use of antibiotics and physiotherapy and are in communication with various stake holders of the multidisciplinary team to achieve the shared goal of day case surgery for all patients undergoing ACL repair.
References
- Vorobeichik L, Brull R, Joshi GP, Abdallah FW. Evidence Basis for Regional Anesthesia in Ambulatory Anterior Cruciate Ligament Reconstruction: Part I-Femoral Nerve Block. Anesth Analg. 2019 Jan;128(1):58-65. doi: 10.1213/ANE.0000000000002854. PMID: 29596099.
- Sehmbi H, Brull R, Shah UJ, El-Boghdadly K, Nguyen D, Joshi GP, Abdallah FW. Evidence Basis for Regional Anesthesia in Ambulatory Arthroscopic Knee Surgery and Anterior Cruciate Ligament Reconstruction: Part II: Adductor Canal Nerve Block-A Systematic Review and Meta-analysis. Anesth Analg. 2019 Feb;128(2):223-238. doi: 10.1213/ANE.0000000000002570. PMID: 29064877.
- Yung EM, Brull R, Albrecht E, Joshi GP, Abdallah FW. Evidence Basis for Regional Anesthesia in Ambulatory Anterior Cruciate Ligament Reconstruction: Part III: Local Instillation Analgesia-A Systematic Review and Meta-analysis. Anesth Analg. 2019 Mar;128(3):426-437. doi: 10.1213/ANE.0000000000002599. PMID: 29200071.
- Ramlogan R, Tierney S, McCartney CJL. Anterior cruciate ligament repair and peripheral nerve blocks: time to change our practice? Br J Anaesth. 2019 Aug;123(2):e186-e188. doi: 10.1016/j.bja.2019.05.028. Epub 2019 Jun 12. PMID: 31202563; PMCID: PMC6676314.
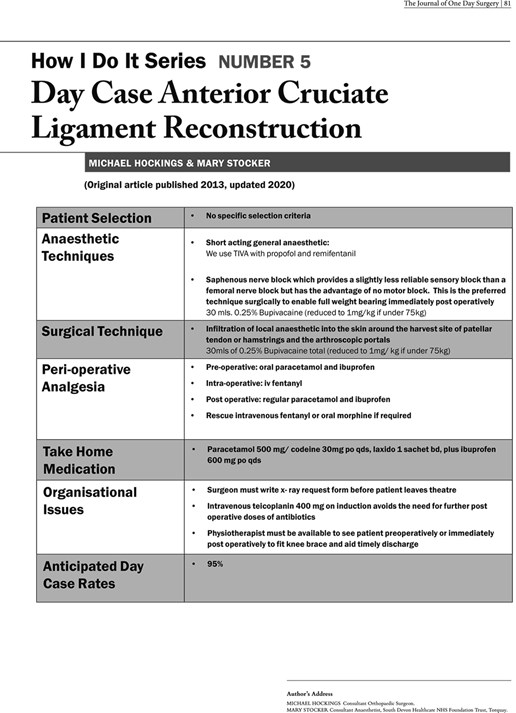
- Hockings M, Stocker M. How I Do It Series: Number 5: Day Case Anterior Cruciate Ligament Reconstruction. J One Day Surg. 2020.
Appendix A
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/51040/312-optimising-anaesthetic-factors-to-facilitate-day-case-anterior-cruciate-ligament-repair.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse8
Dr Laura Wade, Dental Core Trainee 1 laura.wade@mbht.nhs.uk.
Mr N Hampton, Associate Specialist nick.hampton@mbht.nhs.uk
Oral & Maxillofacial Surgery, University Hospitals of Morecambe Bay Acute NHS Trust
Abstract
Introduction: Microcystic Adnexal Carcinoma (MAC) is a rare malignant sweat gland neoplasm. It is slow growing and locally aggressive but rarely metastasises. There have only been a few hundred cases described worldwide (1). During the COVID-19 pandemic, much elective surgery has been postponed, but due to the malignant nature of the lesion, this day case surgery is able to go ahead.
Methods: A 52-year-old female patient presented with a nodular lesion of the right medial eyebrow. Punch biopsy histology described a moderately differentiated squamous cell carcinoma. The lesion was excised and repaired with a local skin flap, and definitive histology reported MAC excised with 3mm margins. The case was discussed at a virtual multi-disciplinary team meeting which advised wider excision. This was undertaken with a supraclavicular full thickness skin graft to cover the defect. Both procedures were carried out as day cases; the patient was tested for COVID-19 and isolated beforehand.
Results: Histology described a highly infiltrative tumour not connecting with the overlying epidermis. It was composed of cords and nests of cells, manifesting ductular and follicular differentiation. The carcinoma invaded subcutaneous fat and perineural tissues. The cells were positive for cytokeratin AE1/AE3 and negative for BerEP4, overall favouring the diagnosis of MAC. Owing to the aggressive potential of this tumour, a wider margin was advised, the result of which was negative for malignancy.
Conclusion: MAC is a malignant tumour which often microscopically exceeds macroscopic margins, and presents clinically as a benign slow-growing lesion. This case follows the treatment of MAC during the COVID-19 pandemic.
Key Words
Microcystic Adnexal Carcinoma; COVID-19; day case
Introduction
Microcystic Adnexal Carcinoma (MAC) is a rare malignant sweat gland neoplasm, which is slow growing and rarely metastasises. Also known as syringomatous carcinoma, malignant syringoma and sclerosing sweat duct carcinoma; there have only been a few hundred cases of MAC worldwide (1). MAC generally occurs in adults aged between 50-60 years old (2), and some literature suggests it has a slight female predilection (3). Typically, MAC presents as a whitish-yellow plaque on the face, and develops a nodular appearance over time, often clinically mimicking Basal Cell Carcinoma (BCC). MAC can occasionally present with altered sensation due to perineural spread (2).
This case follows the treatment of MAC in a 52-year-old female patient as a day case at a North West General Hospital during the COVID-19 global pandemic. Due to the increasing pressures on the NHS, all elective non-cancer surgery was postponed during the height of the pandemic. However, due to the malignant nature of this lesion, surgery was able to go ahead; the patient was tested for COVID-19 and isolated prior to surgery.
Methods
A 52-year-old female patient was referred with a three-month history of a lesion at the right medial eyebrow, which had gradually increased in size. The lesion, which on initial examination appeared benign, was 2 cm in diameter, well defined and nodular in appearance with a pearlescent hue (see Figure 1). Punch biopsy diagnosed a moderately differentiated invasive squamous cell carcinoma (SCC); invading subcutaneous and muscular tissue, at least 4.2mm deep. The patient was informed of the diagnosis and counselled about the invasive and malignant nature of the lesion. Treatment options were discussed and the patient was consented for its surgical removal under local anaesthetic. Medically, the patient was fit and well. She had never smoked and rarely consumed alcohol.
Figure 1. Photograph showing the 2cm, pearlescent nodular lesion which was well defined, with slight induration of the margins and an erythematous base in the right medial eyebrow. Clinically this appeared to be a Basal Cell Carcinoma, but punch biopsy results established an initial diagnosis of SCC. The final diagnosis after excision was Microcystic Adnexal Carcinoma.

University Hospitals of Morecambe Bay Acute NHS Healthcare Trust has three principle hospital sites. The Trust designated Westmorland General Hospital a ‘clean’ hospital where all patients who are admitted would be tested for COVID-19 and asked to isolate for a period of time before the operation. The patient agreed to this protocol, and hence her procedure was able to take place just six days after her initial consultation.
The lesion was excised under local anaesthetic, and the defect repaired with a local ‘A to inverted T’ skin flap (see Figure 2). The suspected SCC was sent to histopathology. The patient was seen a week later in the maxillofacial nurse-led dressings clinic, and the sutures were removed.
Figure 2. Photographs taken during the initial day surgery for removal of the suspected SCC and repair with an ‘A to T’ local skin flap under local anaesthetic. (a) The clinical extent of the lesion is marked (dashed line) and a 6mm margin around the lesion was to be excised. Also note the markings for the ‘A to T’ flap. Photograph (b) shows the wedge of tissue removed, including the lesion itself and excess tissue above the lesion to allow for closure with the local skin flap. The inverted ‘T’ of the flap can be visualised in photograph (c), where the skin flaps either side have been undermined to allow closure. Sutures are placed both deep and superficial, as seen in photograph (d).

Histology reported a highly infiltrative carcinoma composed of narrow cords and nests of relatively bland epidermoid cells which manifested ductular and follicular differentiation. The carcinoma invaded subcutaneous fat and showed not infrequent perineural involvement. There was no clear connection with the overlying epidermis, and the tumour cells were positive for cytokeratin AE1 and AE3, and negative for BerEP4. A DPAS stain showed focal PAS positive material within ductular spaces. The combination of these features favoured a diagnosis of Microcystic Adnexal Carcinoma, rather than the previously described SCC. The carcinoma was clear of the peripheral and deep margins by 3mm.
The case was discussed at the local skin multidisciplinary team meeting, and the regional specialist skin multi-disciplinary team meeting, both of which were held virtually due to the COVID-19 pandemic. They concluded that a wider excision should be undertaken to achieve a 1cm margin of clearance, due to the aggressive potential of the tumour. It was also recommended that the patient undergo Magnetic Resonance Imaging (MRI) of the head and neck, alongside a Computerised Tomography (CT) scan of the thorax, to assess for metastatic disease. These scans were organised, and the secondary procedure was arranged, again following the COVID-19 protocols of testing and isolation prior to day case admission.
The day case surgery was this time completed under a general anaesthetic, due to the patient’s anxieties about the procedure. Further tissue was removed from the right eyebrow, (see Figure 3), and the defect repaired with a full thickness skin graft harvested from the right side of the neck (see Figure 4), cut to size and sutured into the recipient site (see Figure 5). A Proflavine pressure dressing was sutured over the top of the graft (see Figure 6). The patient was discharged home on the day of the surgery, and seen the following week for suture removal.
Figure 3. Photographs taken during the second day case surgery under general anaesthetic. (a) The 2cm in diameter wider local excision of the previously excised MAC is outlined. Note the scars from the previous ‘A to T’ local skin flap repair. (b) The tissue is cut and (c) excised down to the level of the periosteum to ensure clearance. (d) The excised tissue, a marker stitch is placed before the specimen is sent to histopathology for analysis.
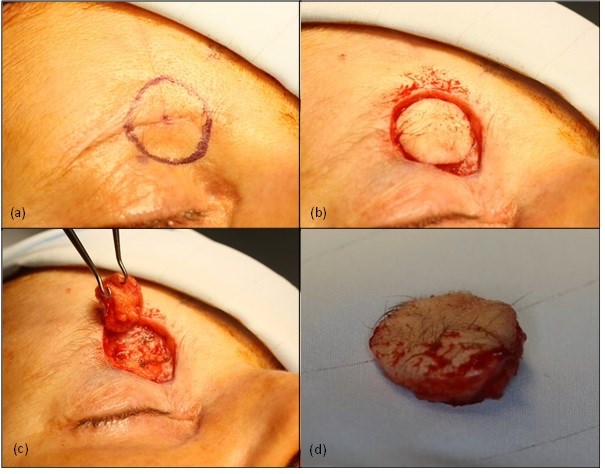
Figure 4. Photographs taken during the second day case surgery under a general anaesthetic. After the wider local excision of the MAC was undertaken (see figure 3), a full thickness skin graft was raised from the right neck. (a) The outline of the skin graft to be harvested. (b) The skin graft mid-way through excision. The skin graft composes of dermis and epidermis; any yellow fat cells are trimmed from the graft. (c) The neck wound is closed with deep and superficial sutures, and the scar is placed in a natural neck crease to reduce aesthetic disturbance.
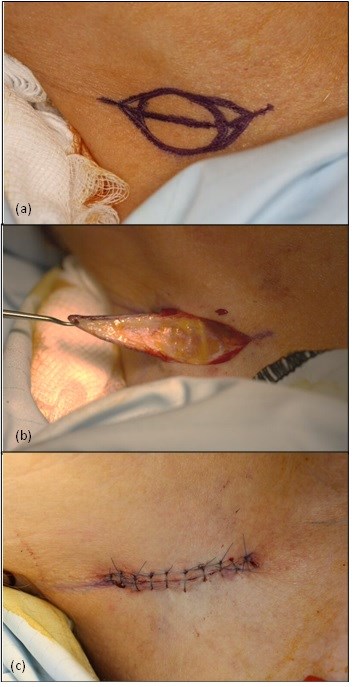
Figure 5. (a) The trimmed graft is placed into the defect, and (b) sutured in place with non-resorbable skin sutures. Quilting stitches are placed in the centre of the graft to hold the graft down to the underlying periosteum and encourage blood supply to the graft.
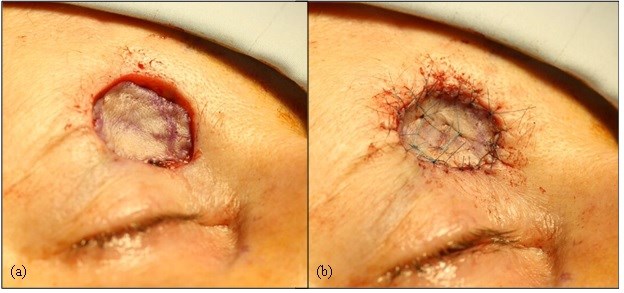
Figure 6. Final photograph of the second day case surgery. The graft is covered by cotton wool balls soaked in Proflavine bacteriostatic disinfectant and sutured into place with non-resorbable tie-over sutures.

Results
Both MRI and CT scans were clear of any metastases or lymphadenopathy, and the wider local excision demonstrated dermal scarring and a foreign body giant cell response, in keeping with the effects of previous surgery at this site. There was no evidence of residual malignancy. The surgical site has healed well (see Figure 7).
Figure 7. Photograph taken by the patient ten weeks after wider local excision of MAC and repair with full thickness skin graft from the right neck (14 weeks post initial surgery). The patient has been advised to continue to moisturise and massage the area to reduce scarring

The patient has been reassured and will now be reviewed according to our local SCC follow-up protocol, attending three-monthly appointments for the first year, four-monthly for the second year and six-monthly for the third year. The patient has been counselled regarding the importance of sun care, self-examination and urgent presentation should she be suspicious of any new or recurring lesions.
Discussion
First described by Goldstein et al in 1982 (4), MAC is a rare malignancy characterised by a pale, firm papule, plaque or nodule which is slow growing and usually asymptomatic (5). Most commonly presenting in females of the sixth decade, risk factors for MAC include but are not limited to: ultraviolet radiation, previous radiation therapy, and immunosuppressive medications (2).
MAC is often clinically overlooked or misdiagnosed, the non-sinister looking white to pink pale plaque on the face is commonly misinterpreted as a BCC, SCC, desmoplastic trichoepithelioma, trichoadenoma or syringoma (6). Originating in the pluripotent adnexal keratinocyte cell, MAC is capable of both follicular and sweat gland differentiation (7).
The misdiagnosis of MAC has also been reported, as in this case, to occur at a histopathological level after biopsy. A study in 2000 of 48 patients demonstrated that 13 (27%) had been incorrectly diagnosed at initial biopsy. The microscopic appearance of MAC is often relatively bland, especially when the biopsy is a superficial punch or shave sample, making pathological identification difficult (8).
The microscopic margins of MAC often extend far beyond the macroscopic margins, making clearance of the lesion a surgical challenge. Many surgeons choose to use Mohs micrographic surgery (MMS) to identify the extent and excise the lesion, which has been shown to be superior with respect to the number of procedures required for total excision: The 2000 study of 48 cases showed that 30% of patients with simple excision at onset will require at least one other procedure compared with as little as 0% if treated with MMS (8). The defects created by total excision with clear margins can be up to six-times the size of the initial clinical lesion (9). The extent of the defect in comparison to the original lesion can be visualised in Figure 8.
Figure 8. A comparison of the lesion before the procedures and the skin graft 4 weeks after the second day case surgery. Note the size difference between the two.

MAC is most commonly confined to skin, however there have been reports of metastasis to the lymph nodes, lungs and mediastinum (10,11), hence the need for MRI and CT imaging in this case. More commonly however is local invasion, into underlying soft tissue, bone and muscle.
Despite the low risk of metastasis, there is a considerable risk of local recurrence of MAC. Cases of recurrence have been reported up to 30 years after the primary tumour was excised (12). Tumours which have not been adequately cleared are at a greater risk of recurrence (9), hence the advised 1cm margin of clear tissue in our reported case, which was achieved following the second day case procedure.
Conclusion
MAC is a malignant, locally aggressive tumour which is commonly misdiagnosed due to its benign façade and slow growing behaviour, along with a bland histological picture. The tumour often microscopically exceeds macroscopic margins, presenting problems with complete excision and recurrence. This case follows the treatment of MAC during the COVID-19 pandemic over two-day case sessions, each carried out at in a North West Hospital Trust, with the appropriate COVID precautions and isolation procedures.
References
- Lopez, Mariela MD; Cole, Eric L. MD Microcystic Adnexal Carcinoma, Plastic and Reconstructive Surgery Global Open: November 2014 - Volume 2 - Issue 11 - p e254
- Zito PM, Mazzoni T. Microcystic Adnexal Carcinoma. [Updated 2020 Sep 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557857/
- Gordon S, Fischer C, Martin A, Rosman IS, Council ML. Microcystic Adnexal Carcinoma: A Review of the Literature. Dermatol Surg. 2017 Aug;43(8):1012-1016.
- Gerall, C., Sippel, M., Yracheta, J. and Hogan, F., 2019. Microcystic Adnexal Carcinoma: A Rare, Commonly Misdiagnosed Malignancy. Military Medicine, 184(11-12), pp.948-950.
- Calderón-Castrat, X., Román-Curto, C., Santos-Briz, A. and Fernández-López, E., 2017. Microcystic adnexal carcinoma mimicking basal cell carcinoma. JAAD Case Reports, 3(6), pp.492-494.
- Zhang, L., Huang, X., Zhou, T. and Cao, H., 2020. Microcystic adnexal carcinoma: report of rare cases. Bioscience Reports, 40(1).
- Goldstein, D., Barr, R. and Cruz, D., 1982. Microcystic adnexal carcinoma: A distinct clinicopathologic entity. Cancer, 50(3), pp.566-572.
- Chiller K, Passaro D, Scheuller M, Singer M, McCalmont T, Grekin RC. Microcystic Adnexal Carcinoma: Forty-eight Cases, Their Treatment, and Their Outcome. Arch Dermatol.2000;136(11):1355–1359. doi:10.1001/archderm.136.11.1355
- Hamed, N. and Khachemoune, A., 2015. Microcystic adnexal carcinoma: A focused review and updates. Journal of Dermatology & Dermatologic Surgery, 19(2), pp.80-85.
- Ban M, Sugie S, Kamiya H, Kitajima Y. Microcystic adnexal carcinoma with lymph node metastasis. Dermatology. 2003;207(4):395-7. doi: 10.1159/000074122. PMID: 14657634.
- medscape.com. 2021. Microcystic Adnexal Carcinoma: Practice Essentials, Background, Pathophysiology. [online] Available at: <https://emedicine.medscape.com/article/1101894-overview> [Accessed 24 February 2021].
- Lupton, G., 1986. Microcystic adnexal carcinoma. Report of a case with 30-year follow-up. Archives of Dermatology, 122(3), pp.286-289.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/51041/312-treatment-of-microcystic-adnexal-carcinoma.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse9
Click on the image to be taken to the HCUK page about the conference.
Download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50106/hcc-bads-general-surgery-18_06_2021.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse10
Click on the image to be taken to the HCUK page about the conference.
Download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50104/hcc_bads-day-surgery-gynaecology-20_05_2021.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse11
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/50105/bads-day-surgery-urology-jul-2021.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse12
General Guidelines
The Journal of One-Day Surgery considers all articles of relevance to day-surgery and short-stay surgery. Articles may be in the form of original research, review papers, audits, service improvement reports, case reports, case series, practice development and letters to the editor. Research projects must clearly state that ethics committee approval was sought where appropriate and that patients gave their consent to be included. Patients must not be identifiable unless their written consent has been obtained. If your work was conducted in the UK and you are unsure as to whether it is considered as research requiring approval from an NHS Research Ethics Committee (REC), please consult the NHS Health Research Authority decision tool at http://www.hra-decisiontools.org.uk/ethics/.
Articles should be prepared as Microsoft Word documents with standard line spacing and normal margins. Submissions must be sent by email to the address below.
Copyright transfer agreement and submission
https://daysurgeryuk.net/en/resources/documentation/
Each named author should complete and sign a copy. Scanned copies/legible photos should be sent via email together with the main manuscript to the JODS editor: davidbunting@nhs.net
Any source of funding should be declared, and authors should also disclose any possible conflict of interest that might be relevant to their article.
Submissions are subject to peer review. Proofs will not normally be sent to authors and reprints are not available.
Manuscript preparation
Title Page
Abstract
An abstract of 250 words maximum summarising the manuscript should be provided and structured as follows: Introduction, Methods, Results, Conclusions.
Main article structure
Tables, Figures and Graphs
Please submit any figures, graphs and images as separately attached files rather than embedding non-word files into the word manuscript document. Tables constructed in MS Word can be left in their original MS Word file including the manuscript if this is where they were drawn.
Figures and graphs can be presented in colour but try to avoid 3-d effects, shading etc. Figures and graphs may be redrawn if the quality is not in keeping with the Journal. Please make it clear within the manuscript text where you would like tables, graphs or images to be placed in the finished article with the use of a brief explanatory legend in the manuscript file where you wish the item to be placed, e.g.
Table 1. Patient demographic details.
Figure 1. Proportion of procedures performed as a day-case each year between 2005 and 2018.
Photographs
References
Please follow the Vancouver referencing style:
- References in the reference list should be cited numerically in the order in which they appear in the text using Arabic numerals, e.g. 1, 2, 3, 4 etc.
- The reference list should appear at the end of the paper. Begin your reference list on a new page and title it 'References.'
- Cite articles in the manuscript text using numbers in parentheses and the end of phrases or sentences, e.g. (1,2)
- Abbreviate journal titles in the style used in the NLM Catalogue: https://www.ncbi.nlm.nih.gov/nlmcatalog?Db=journals&Cmd=DetailsSearch&Term=currentlyindexed%5BAll%5D
- The reference list should include all and only those references you have cited in the text. (However, do not include unpublished items such as correspondence).
- Check the reference details against the actual source - you are indicating that you have read a source when you cite it.
- Be consistent with your referencing style across the document.
Example of reference list:
- Ravikumar R, Williams J. The operative management of gallstone ileus. Ann R Coll Surg Engl 2010;92:279–281.
- Dybvig DD, Dybvig M. Det tenkende mennesket. Filosofi- og vitenskapshistorie med vitenskapsteori. 2nd ed. Trondheim: Tapir akademisk forlag; 2003.
- Beizer JL, Timiras ML. Pharmacology and drug management in the elderly. In: Timiras PS, editor. Physiological basis of aging and geriatrics. 2nd ed. Boca Raton: CRC Press; 1994. p. 279-84.
- Kwan I, Mapstone J. Visibility aids for pedestrians and cyclists: a systematic review of randomised controlled trials. Accid Anal Prev. 2004;36(3):305-12.
- Barton CA, McKenzie DP, Walters EH, et al. Interactions between psychosocial problems and management of asthma: who is at risk of dying? J Asthma [serial on the Internet]. 2005 [cited 2005 Jun 30];42(4):249-56. Available from: http://www.tandf.co.uk/journals/.
Mr David Bunting
Editor, Journal of One Day Surgery
British Association of Day Surgery
Consultant Upper GI Surgeon
North Devon District Hospital
[These guidelines were last revised on 14.04.2021]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/51042/312-author-guidelines.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2198#collapse13